Introduction
Bone and joint health form the structural and functional core of lifelong mobility, physical independence, and overall quality of life. Yet, they are often overlooked until significant loss or dysfunction occurs. For women in particular, the interplay between hormones, nutrition, and physical activity makes skeletal health especially vulnerable across the life course, from adolescence through post-menopause.
Bones are dynamic, living tissue that constantly undergo a process of remodelling where old bone is broken down (resorption) and replaced with new tissue (formation). However, this balance shifts unfavourably with age, hormonal changes, and lifestyle factors. By the time symptoms such as joint stiffness or poor flexibility emerge, significant underlying deterioration may already be underway.
Why Women Need to Prioritise Bone and Joint Health Early
Peak bone mass (an individual’s maximum bone strength and density) is typically achieved by the late 20s. After this point, bone breakdown gradually begins to exceed formation, making the early adult years a critical period for optimising skeletal health. For women, this is especially important due to the protective role of oestrogen in bone remodelling. Oestrogen suppresses bone resorption and promotes collagen production, essential for both bone density and joint integrity.
During perimenopause and menopause, oestrogen levels decline sharply, accelerating bone loss. Women can lose up to 20% of their bone mass within five to seven years of menopause, significantly increasing their risk of osteopenia, osteoporosis, and fragility fractures (Compston et al., 2019). Around 80% of those affected by osteoporosis are women (IOF, 2021). Joints, too, become more susceptible to degeneration as collagen synthesis slows and inflammation rises, impacting flexibility and mobility.
However, the risk trajectory for these conditions begins far earlier than most realise. Nutrition, exercise, and energy availability during adolescence and young adulthood directly shape skeletal resilience later in life. Restrictive diets, low calcium or vitamin D intake, sedentary habits, and chronic stress all impair bone accrual. For younger women, disordered eating patterns or overtraining can disrupt menstrual function and oestrogen production, mimicking menopausal effects on the bones and joints (Mountjoy et al., 2014).
Building Resilience Through Nutrition and Movement
Optimal skeletal health depends on a synergy of nutrients and movement. UK recommendations advise a daily calcium intake of 700–1200 mg depending on age, and a minimum of 10 µg (400 IU) of vitamin D, particularly important in months with low sunlight exposure. Magnesium, vitamin K2, protein, and omega-3 fatty acids also play key roles in maintaining bone mineral density, collagen synthesis, and reducing inflammation around joints.
Physical activity is equally critical. Weight-bearing and resistance training exercises stimulate bone formation and help maintain muscle mass, which supports joints and reduces the risk of falls. Flexibility and mobility practices such as yoga, Pilates, and dynamic stretching not only improve joint range of motion and proprioception but also support postural alignment and recovery. As women age, these practices become vital for maintaining independence and preventing joint deterioration.
Recovery practices, such as sleep, stress management, and soft tissue care should not be underestimated. Chronic sleep deprivation and unmanaged stress elevate cortisol levels, which can accelerate bone resorption and impair connective tissue repair. Structured recovery also helps prevent overuse injuries and preserves joint function over time.
A Lifelong Approach to Bone and Joint Health
It’s never too early, or too late to begin caring for your bones and joints. Prevention during youth builds stronger foundations, while targeted interventions in adulthood and beyond can slow degeneration, enhance recovery, and preserve mobility.
Across the life stages, consistent attention to dietary quality, physical activity, recovery, and screening can dramatically alter the trajectory of musculoskeletal ageing. Whether you’re an active young adult, approaching midlife changes, or navigating post-menopausal transitions, investing in bone and joint health is essential for maintaining the freedom to move well, age well, and live well.
What Is Bone Density and When Should You Check It?
Bone density is a measure of the strength and mineral content of bones, most commonly assessed using DEXA scans. It’s advisable for women to consider a bone density test:
- If there's a family history of osteoporosis
- If they have had frequent fractures
- If entering perimenopause (often around age 40+)
- If following restrictive diets or underweight (BMI < 18.5)
- If diagnosed with conditions like coeliac disease, PCOS, or amenorrhoea
What Our Nutritionist Recommends
Key Nutrients for Bone & Joint Health
- Calcium: 1000–1200 mg/day from food and supplements
- Vitamin D3: 1000–2000 IU daily for absorption and hormone regulation
- Magnesium: 320 mg/day to support calcium balance and muscle function
- Vitamin K2: Directs calcium to bones, not arteries
- Collagen peptides: May improve bone mineral density and joint cartilage (König et al., 2018)
- Boron: Supports hormone levels and mineral metabolism
- Isoflavones (soy, flax): Help preserve bone during oestrogen loss
Lifestyle Essentials
- Resistance and weight-bearing exercise: e.g., squats, walking, resistance bands
- Mobility and stretching e.g., yoga, swimming, Pilates
- Limit alcohol and smoking: Both are major bone risk factors
- Get sunlight exposure: 10–15 minutes daily for vitamin D production
Recommendations from Nutritionists
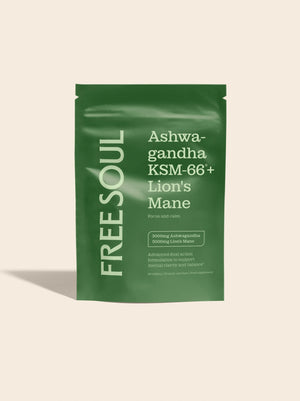
- Free Soul Female Multivitamin with Collagen: Helps maintain bone mineralisation and calcium absorption.
- Free Soul Marine Collagen (with Hyaluronic Acid & Vitamin C): Collagen supports joint tissue, cartilage integrity, and skin elasticity. Vitamin C boosts natural collagen synthesis.
- Free Soul Vegan Protein Blend (with added vitamins & minerals): Provides plant-based protein to support muscle around joints, plus added nutrients like magnesium and calcium for bone health.
- Free Soul 4-in-1 Magnesium + Turmeric: Magnesium is essential for calcium absorption and bone mineralisation.